General Health Tips & News
Diabetic Ketoacidosis, All you need to know about DKA
By A.S. (staff writer) , published on November 03, 2020
Medicine Telehealth Health DKA Hyperglycemia Osmotic diuresis
Diabetic ketoacidosis (DKA) is an acute, major, life-threatening complication of diabetes characterized by hyperglycemia, ketones bodies’ formation, and osmotic diuresis that leads to significant fluid and electrolyte loss.
It can happen when your high blood sugar level remained untreated for a long time. DKA happens when your blood sugar is very high and acidic substances called ketones build up to dangerous levels in your body.
DKA occurs mainly in patients with type 1 diabetes, but it is not uncommon in some patients with type 2 diabetes. DKA only appears when your body does not have enough insulin to process high levels of glucose in the blood.
It’s less common in people with type 2 diabetes because insulin levels don’t usually drop so low; however, it can occur. DKA may be the first sign of type 1 diabetes, as people with this disease can’t make their own insulin.
Pathophysiology:
DKA usually happens because your body doesn't have enough insulin. Without insulin, your body can’t utilize glucose for its energy purposes; your body begins to break down fat (lipolysis) in an attempt to get the energy it needs, a process that ultimately results in a dangerous buildup of acids, known as ketones, in your bloodstream. When ketones build up in the blood, they make it more acidic.
Insulin prevents ketogenesis (ketones bodies’ formation) by inhibiting the transport of free fatty acids into the matrix of mitochondria. Beta-oxidation of fatty acids produces acetone, acetoacetic acid, and beta-hydroxybutyrate, which causes metabolic acidosis.
Hyperglycemia with ketones due to insulin deficiency causes an osmotic diuresis that leads to marked urinary losses of fluid and electrolytes. Urinary excretion of ketones further causes the loss of potassium and sodium. If the serum potassium level is not monitored and replaced as needed, life-threatening hypokalemia may develop.
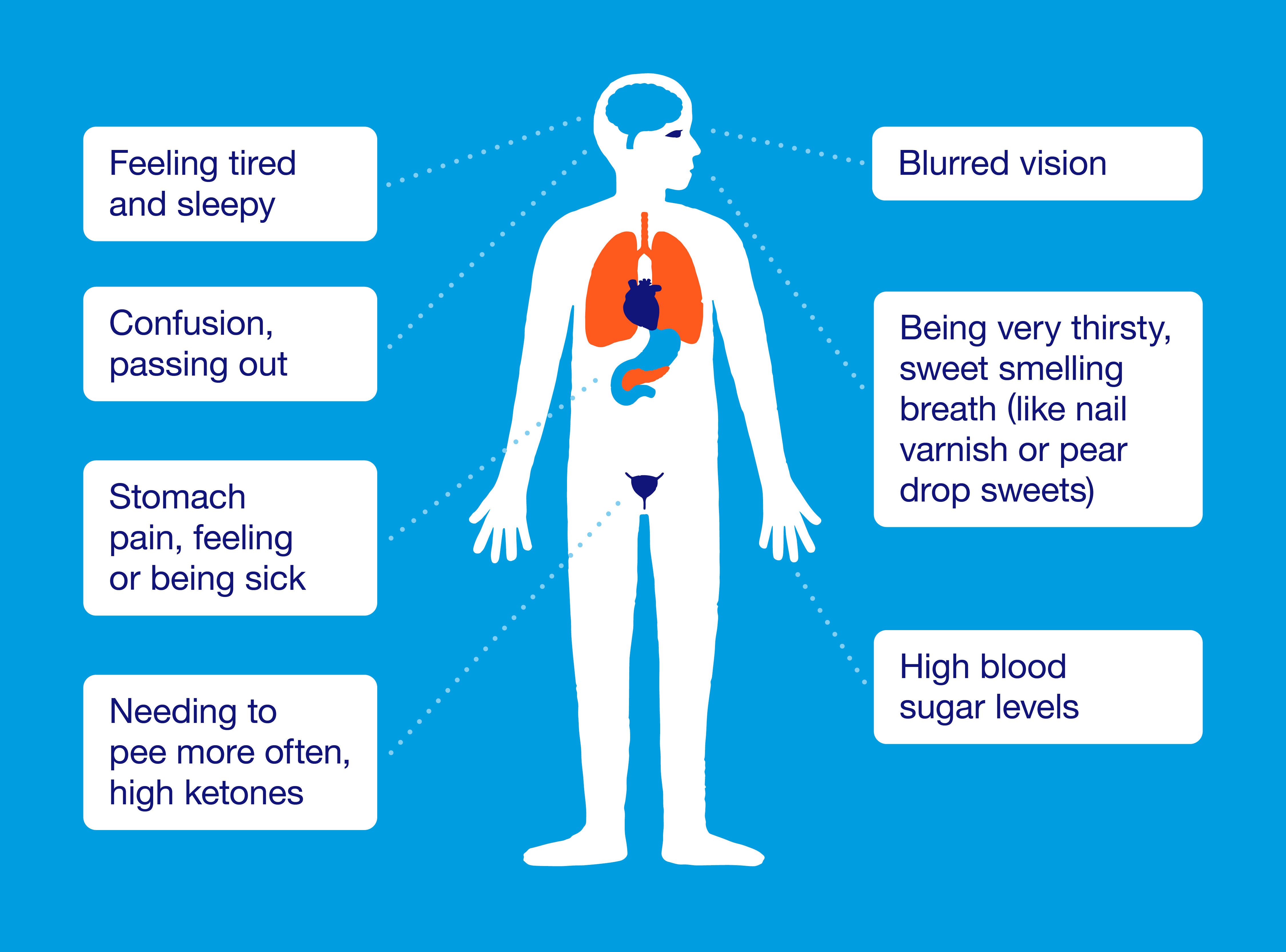
Signs and Symptoms:
Early symptoms of DKA include;
-
Thirst or a very dry mouth
-
Lethargy and feeling sleepy
-
Frequent urination
-
High blood glucose (blood sugar) levels (hyperglycemia)
-
High levels of ketones in the urine
-
Confusion
-
Stomach pain, feeling or being sick
-
Needing to pee more often
-
Patients may be hypotensive and tachycardic due to dehydration and acidosis.
-
Fruity breath due to exhaled acetone.
Diagnosis
Diagnosis of DKA includes:
-
Hyperglycemia
-
Arterial pH
-
Blood urea nitrogen (BUN), serum creatinine.
-
Serum ketones
-
Anion gap
DKA is diagnosed by an arterial pH < 7.30 with an anion gap > 12 and serum ketones in the presence of hyperglycemia.
Causes of DKA:
The most common causes of DKA include:
-
Missing an insulin injection or not injecting enough insulin
-
Missing meals
-
Insulin reaction
-
Illness or infection
Treatment:
The main goal is to keep the high blood glucose level within check (hyperglycemia), the reversal of acidosis and ketosis, replenishment fluid losses, and electrolytes due to osmotic diuresis. The identification of underlying factors is also important.
Fluid replacement:
To compensate for fluid loss through osmotic dieresis, intravascular fluid (IV saline 0.9 %) 1-3 liters given to raise blood pressure and ensure glomerular perfusion and dehydration.
Correction of hyperglycemia and acidosis:
Hyperglycemia is corrected by giving regular insulin 0.1 unit/kg IV bolus initially, followed by continuous IV infusion of 0.1 unit/kg/hour in 0.9% saline solution. Ketones start to wipe off within hours if insulin is given in sufficient doses.
Bicarbonate administration is considered if the pH of blood is less than 7 about an hour of initial fluid replenishment.
When plasma glucose becomes < 200 mg/dL in adults, 5% dextrose should be added to IV fluids to reduce the risk of hypoglycemia.
Manage Hypokalemia
Hypokalemia management requires replacement of 20 to 30 mEq potassium in each liter of IV fluid to keep serum potassium between 4 and 5 mEq/L.
Prevention:
Steps should follow to avoid DKA
-
Monitor blood sugar levels.
-
Check your ketone levels
-
Take medications regularly as prescribed
-
Keep yourself hydrated
-
Adjust the insulin dosage as needed.
References
- Deborah Weatherspoon, P. R. (2020, May 7). What You Should Know About Diabetic Ketoacidosis. Retrieved from Healthline: https://www.healthline.com/health/type-2-diabetes/ketoacidosis
- DKA (Ketoacidosis) & Ketones. (n.d.). Retrieved from American Diabetes Association: https://www.diabetes.org/diabetes/complications/dka-ketoacidosis-ketones
- Erika F. Brutsaert, M. (2020, September). Diabetic Ketoacidosis (DKA). Retrieved from MSD Manuals: https://www.msdmanuals.com/professional/endocrine-and-metabolic-disorders
- Henriksen, K. (2020, September 10). What Is Diabetic Ketoacidosis? Retrieved from Endocrineweb: https://www.endocrineweb.com/diabetic-ketoacidosis
- Osama Hamdy, M. P. (2019, May 19). Diabetic Ketoacidosis (DKA) Treatment & Management. Retrieved from Medscape: https://emedicine.medscape.com/article/118361-treatment
Find articles related to: Medicine Telehealth Health DKA Hyperglycemia Osmotic diuresis
More articles about General Health Tips & News
Back to the Health Tips Index




