Digestive System
Esophageal Varices: What are its Symptoms, Causes, and Treatment?
By S.I. (staff writer) , published on December 29, 2023
Medicine Telehealth Health bleeding hypertension
What are Esophageal Varices?
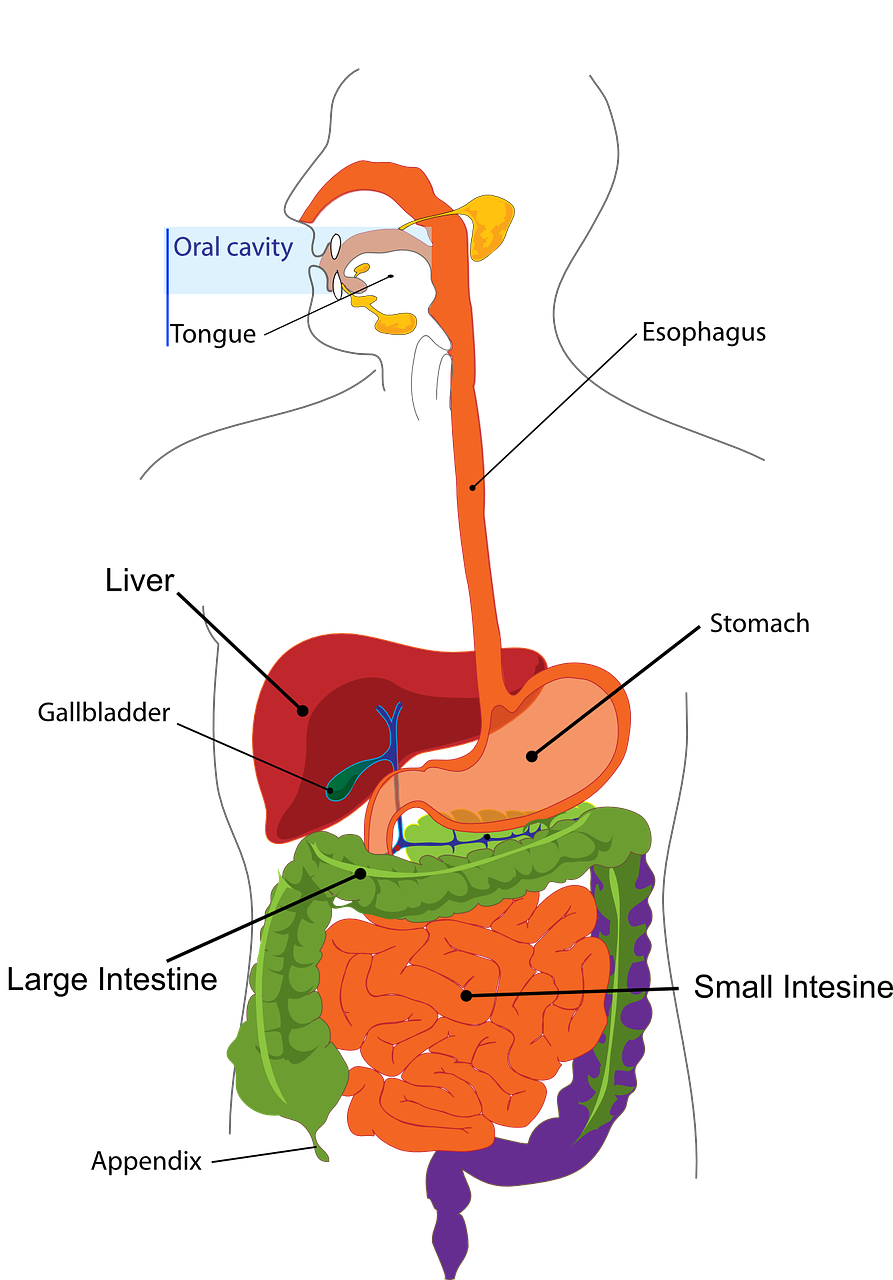
Varices are dilated blood vessels. The esophagus is a tube that attaches the mouth to the stomach. Enlarged blood vessels in the esophagus are known as esophageal varices [1]. It is associated with liver diseases, most commonly liver cirrhosis. Esophageal varices develop when any clot or scar tissue in the liver obstructs blood flow to the liver.
To overcome the blockage and supply blood to the desired organ, large volumes of blood flow through a small blood vessel. The small blood vessels can eventually leak or even burst, resulting in bleeding, often life-threatening.
What are the Symptoms of Esophageal Varices?
The most important symptom of esophageal varices is gastrointestinal bleeding [2]. Other symptoms are as follows:
- Hematemesis (Blood Vomiting)
- Melena (black stool due to upper gastrointestinal tract bleed)
- Hematochezia is the passage of fresh blood through the anus, usually in or with stool. It is an indication of acute gastrointestinal bleeding. [3]
- Undiagnosed Cirrhosis
- Weight loss in patients with chronic liver diseases
- Alcohol
- Exposure to blood-borne viruses
- Jaundice
- Abdominal pain
- Anorexia
- Pruritus
- Muscle Cramps
- Altered mental status
- Easy bleeding or bruising
- Splenomegaly
- Ascites
What are the Causes of Esophageal Varices?
The leading cause of esophageal varices is portal hypertension. Esophageal varices are formed when blood flow to the liver is blocked usually by scar tissue in the liver also known as Cirrhosis. [4]
Because of portal hypertension, the blood seeks alternative pathways through smaller veins such as those in the lowest part of the esophagus. These thin-walled veins swell with the additional blood and may rupture and bleed.
The potential causes of portal hypertension are as follows:
- Pre-hepatic: portal vein obstruction and splenomegaly with increased splenic vein blood flow.
- Post-hepatic: the cause is not related to the liver itself. That may be severe right-sided heart failure, pericarditis, and hepatic vein obstruction.
- Intra-hepatic: The most common intrahepatic cause of portal hypertension is Cirrhosis.
Some other causes include parasitic infections most importantly, schistosomiasis. Blood clots, also known as thrombus in the portal vein or splenic vein can also cause esophageal varices.
Diseases that can affect portal microcirculation, e.g. nodular regenerative hyperplasia and diffuse fibrosing granulomatous diseases such as sarcoidosis can also cause portal hypertension and hence, esophageal varices.
What are the Treatment Options for Esophageal Varices?
The treatment aims to prevent bleeding from the gastrointestinal tract. The following approaches are considered while treating esophageal varices [5]:
- Banding
- Sclerotherapy
- Transjugular Intrahepatic Portosystemic Shunt (TIPS)
- Distal Splenorenal shunt (DSRS)
- Liver Transplant
- Revascularization
- Esophageal transection
References:
- https://medlineplus.gov/ency/article/000268.htm
- https://www.ncbi.nlm.nih.gov/books/NBK448078
- https://www.ncbi.nlm.nih.gov/books/NBK411/#:~:text=Hematochezia%20is%20the%20passage%20of,usually%20in%20or%20with%20stools.
- https://www.mayoclinic.org/diseases-conditions/esophageal-varices/symptoms-causes/syc-20351538
- https://www.webmd.com/digestive-disorders/bleeding-varices
Find articles related to: Medicine Telehealth Health bleeding hypertension
More articles about Digestive System
Back to the Health Tips Index




